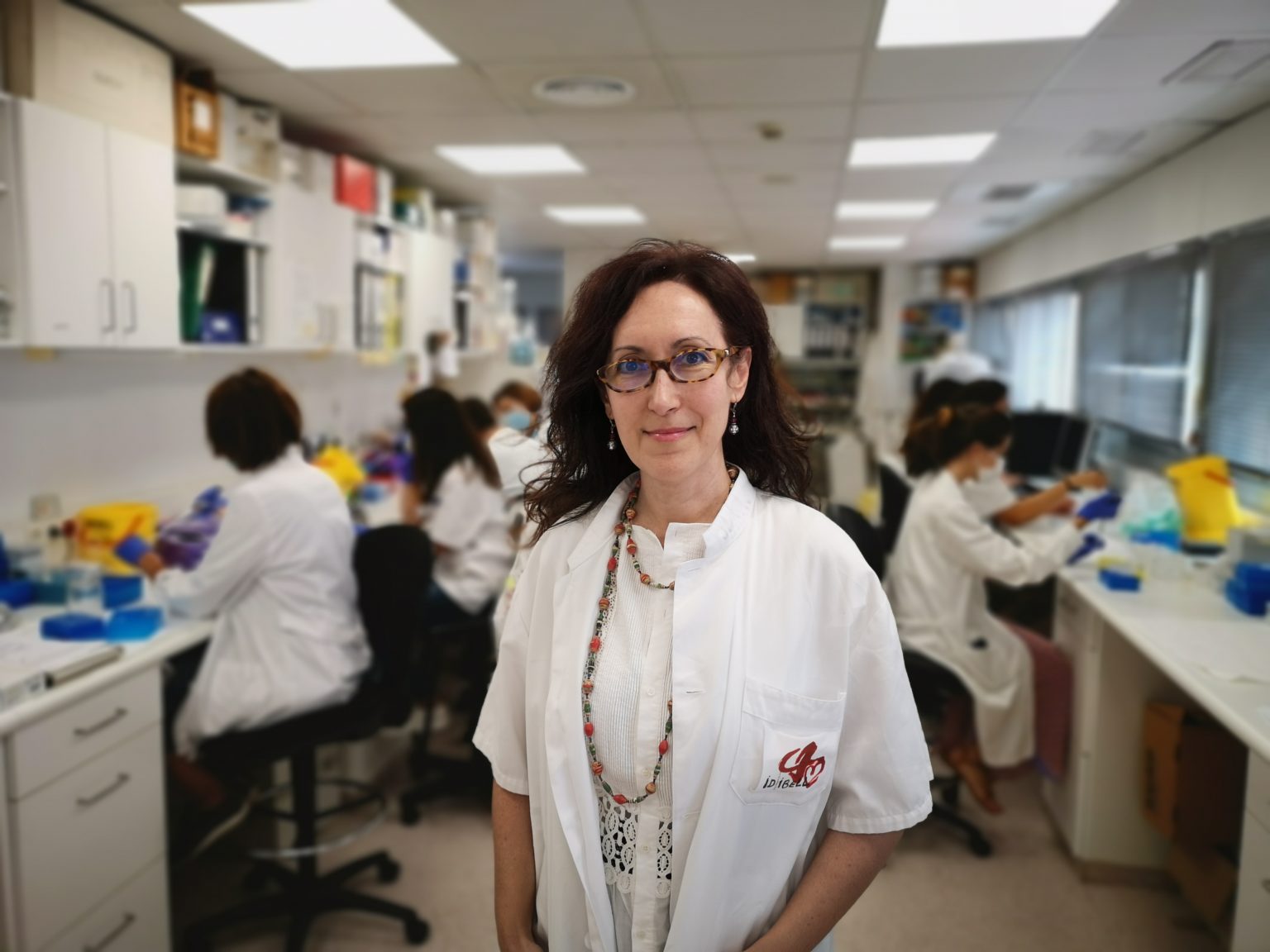
BCN, 25 Sept, 2020.- Age, sex, and the presence of previous pathologies are the main factors associated with a worse prognosis for COVID-19, but the causes that lead young people without comorbidities to develop severe forms of the disease are still unknown. In two articles published today in the journal Science researchers identify alterations of interferon and the proteins of its signaling pathway as predictive markers of severity in these individuals. Dr. Aurora Pujol, geneticist and ICREA professor at the Bellvitge Biomedical Research Institute (IDIBELL), participated in the study and involved the CNAG-CRG that was in charge of analyzing the genome of COVID-19 patients through the EU-funded project EASI-Genomics.
The international consortium Covid Human Genetic Effort, led by the Rockefeller University of New York, has analysed the genomes of 659 severe COVID-19 patients and has found a high frequency of mutations that would affect the levels of interferon and the proteins of the lung cells responsible for its activity. Specifically, genetic alterations have been detected in eight genes important in the immune response against viruses, while a similar group of asymptomatic or mild patients did not have these mutations.
Knowing the importance of these alterations in the evolution of the disease can become an important therapeutic and preventive tool since it will be very useful for the selection of the population at risk of developing severe pneumonia, which will facilitate the screening of patients who require a special care and priority access to artificial ventilation or the ICU.
“Now that we know one of the molecular causes of why some young people develop severe forms of the disease, we can fine-tune our therapeutic options, such as interferon treatment,” says Dr. Aurora Pujol.
This list of mutations, which could also be relevant in other viruses, is likely to expand as more cases are studied.
“COVID-19 patients with a worse prognosis who do not have any of these alterations may have a previous undiagnosed pathology or other genetic susceptibilities that cause an incorrect immune response,” explains Pujol.
Interferons are hormone-like signalling proteins that are essential in the body defence against viral infections. This type of immune response is even more important in the fight against the SARS-CoV-2 virus, since the virus itself has mechanisms to reduce the production of interferon by the cells of the immune system. Therefore, in people with these mutations, the effects would add up and the virus would go unnoticed by the body’s defences.
The results are the fruit of a collaboration between hundreds of hospitals that were collecting samples in the harshest moments of the first wave of the pandemic and of researchers who have sequenced and analysed the data even from the lockdown. Apart from IDIBELL, this study has also had the participation of specialists from the Vall d’Hebron Research Institute (VHIR).
On the other hand, the CNAG-CRG provided genome analysis of COVID-19 patients through the EU-funded project EASI-Genomics, that CNAG-CRG coordinates. The unit led by Marta Gut delivered clinical grade next-generation sequencing with rapid turn-around which is critical in a pandemic. Illumina provided Matched Funding for the COVID-19 projects.
Autoantibodies against interferon
The genetic results are complemented by those of a second study also published today in Science and where scientists from the same consortium, in this case with the participation of IDIBELL and the IrsiCaixa AIDS Research Institute, have found that many of these young patients who develop a severe form of COVID-19 would be generating antibodies against their own interferon. This phenomenon would reduce the activity of the cytokines produced, causing an effect similar to that of the mutations described in the first article.
Therefore, the two studies would reinforce the importance of interferon in the immune response against the coronavirus since deficiencies in its functioning, whether genetic or due to the generation of autoantibodies, would be behind at least 15% of severe pneumonias. However, this number may increase in the future when studying other elements involved in this type of immune response or its antagonistic pathways, which could be stimulated.
Genomic medicine in pandemic management
The study of atypical cases, whether they are elderly individuals who are asymptomatic or even do not become infected despite being exposed to the virus, or young healthy patients at risk of losing their lives, is an opportunity to find the molecular causes and genetic biomarkers that give us clues about the evolution of the infection and the prognosis of each patient, while helping us to understand the immune response to this and other infections.
Knowing the individual conditions that determine clinical variability opens up new ways to study infectious diseases and to better control pandemics. In this sense, both the genetics of the host and the possible variations of the virus and the viral load at the time of infection are key to determining the severity of the disease. Personalized medicine can provide solutions to detect these individuals at higher risk, and to develop and implement more targeted treatments.
“These articles are an example of the wide range of applications that the latest biomedical revolution, genomic medicine, has and is an example of its transversality“, says Pujol. “Our group has a long history in the study of genetic brain diseases, but the social and health crisis caused by the pandemic has pushed us to redirect efforts and adapt our genomic analysis algorithms to be able to study the immune response to this new virus. It is an opportunity to learn; and a good example of networking at a global level that will help to overcome this crisis and to be better prepared for future pandemics”.
Works of reference
Inborn errors of type I IFN immunity in patients with life-threatening COVID-19
Auto-antibodies against type I IFNs in patients with life-threatening COVID-19
(Text slightly adapted from the IDIBELL press release)