Barcelona, 5th of October, 2022.- Researchers from IDIBAPS have coordinated a study to identify the mechanisms that determine the evolution of leukaemia, how relapse occurs after treatment and how, in some patients, it transforms into a very aggressive lymphoma at the final stage of the disease.
The study, published in the journal Nature Medicine, and financed with a grant from the CaixaResearch call for health research of one million euros, shows that the cells that cause relapse after treatment - and which will also transform leukaemia into a highly aggressive tumour – can already be detected in very small amounts at the beginning of the disease, many years before these complications become clinically apparent. The results of this work change the view of how leukaemia progresses.
The article has been coordinated by Dr. Elías Campo, Director of IDBAPS, Head of the Molecular Pathology of Lymphoid Neoplasms group and Head of the CIBERONC group, and Dr. Ferran Nadeu, Postdoctoral Researcher at IDIBAPS and CIBERONC. The first co-authors of the work are, in addition to Ferran Nadeu, Romina Royo, researcher at the Barcelona Supercomputing Center – Centro Nacional de Supercomputación (BSC-CNS); Ramon Massoni-Badosa, researcher at the Centro Nacional de Análisis Genómico (CNAG-CRG); Heribert Playa-Albinyana, IDIBAPS and CIBERONC researcher; and Beatriz Garcia-Torre, IDIBAPS researcher.
The Big Bang Theory of Cancer Evolution
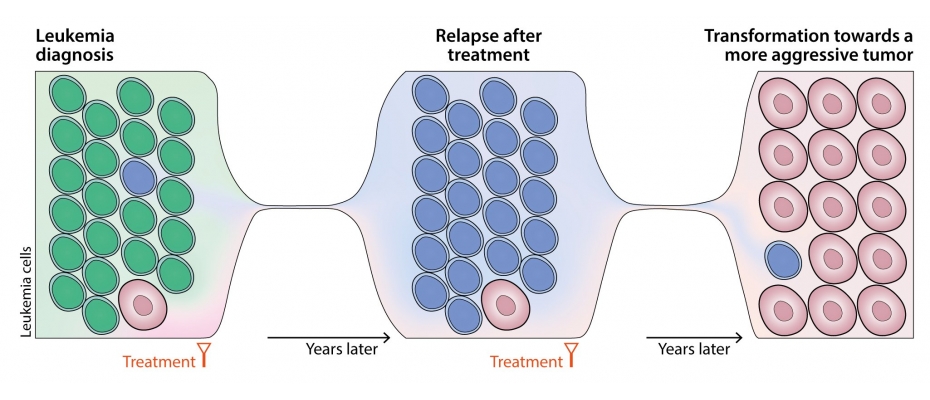
Until now, it was thought that leukaemia progressed because its cells evolved over time, becoming more aggressive tumours because they progressively acquired alterations in their genome that made them more resistant to treatment. The new work shows that some of the leukaemia cells have already acquired these alterations at the beginning of the disease, but they are found in very small quantities. During the evolution of the disease, these more malignant cells will increase and will progressively be selected to cause clinical complications many years after their onset.
“It is as if the stem cell of leukaemia engenders many daughter seeds since the beginning of the disease, each one of them with different alterations that will allow them to grow in the future when the conditions are more suitable”, says Elías Campo.
These observations confirm the so-called "Big Bang" theory of cancer evolution, which proposes that the original malignant cell rapidly multiplies into a large number of very diverse daughter cells with multiple alterations that give rise to future complications through a process of cell selection of the most adapted.
"This new view of the disease opens the door to developing highly sensitive diagnostic tests that allow us to detect and treat these malignant seeds many years before they can grow uncontrollably," explains Elías Campo.
The transformation of chronic lymphatic leukaemia into a more aggressive tumour
Chronic Lymphocytic Leukaemia (CLL) is the most common leukaemia in the Western world, with a prevalence of around 5 cases per 100,000 inhabitants per year. It is usually indolent, but it can evolve into a very aggressive large B-cell lymphoma with a median survival of less than one year. This tumour transformation occurs in approximately 5-10% of patients.
For the study in Nature Medicine, the researchers set out to study in depth the alterations that determine the progression of leukaemia using blood samples obtained at different times of the disease with new highly sensitive techniques that include individual genome sequencing of thousands of cells tumours at each stage of evolution. Tumour samples were collected from 19 patients with CLL at diagnosis, at relapses after different treatments and until the final moment of transformation to aggressive lymphoma covering up to 19 years after disease onset.
In the study, they identified the genomic alterations that determine progression and, surprisingly, found that a few cells at the earliest stage of the disease already had these alterations.
"Our study highlights that technological advances and potential clinical applications go hand-in-hand. Single-cell genomics has provided us with unprecedented discriminatory power to detect extremely infrequent cancer clones that are key for the prognosis and treatment of Richter's transformation," says Ramon Massoni-Badosa, researcher at the Single Cell Genomics team of the CNAG-CRG.
In addition, alterations in the metabolism of these more aggressive cells were also identified, which, fortunately, seem to be a weakness - an Achilles' heel that could be used to treat or prevent these complications. "We have seen that if we treat the transformed cells with a drug that blocks this metabolism, we markedly reduce their growth," says Ferran Nadeu. This drug is already being tested in clinical trials in patients with other types of leukaemia and solid tumours, and the current study suggests that it could also be used in chronic lymphatic leukaemia.
"This research illustrates how an aggressive transformation occurs in the context of indolent cancer, a phenomenon that could be explored beyond this type of leukaemia," says Elías Campo. "The study shows that single-cell DNA and RNA sequencing is a necessary tool to delve into the biology of cancer and that it will help us diagnose and find new treatments to tackle the disease," he concludes.
The study has been made possible thanks to funding from the European Research Council (ERC) Synergy grant "BCLLatlas" to Elías Campo, Ivo Gut, Iñaki Martín Subero and Holger Heyn, the “la Caixa” Foundation and and the American Association for Cancer Research (AACR), the European Hematology Association (EHA) and the Lady Tata Memorial Trust to Dr. Ferran Nadeu.
Figure
Diagram of the evolution of leukaemia towards a more aggressive tumour. The cells of each colour (green, blue and pink) represent a subpopulation of the tumour. The study identifies how the cells that give rise to relapse after treatment (blue) and the transformation into a more aggressive tumour (pink) were already present at the time of diagnosis in a small amount.
Work of reference
Detection of early seeding of Richter transformation in chronic lymphocytic leukemia
Source: IDIBAPS-Clínic